 Very interesting email I received on one of my favourite topics. If you measure what is going in it strikes me what is coming out is equally important.
Very interesting email I received on one of my favourite topics. If you measure what is going in it strikes me what is coming out is equally important.After our US and India app releases, it has been an interested time!
The absence or relative concentration of different parameters may provide inputs for healthcare professionals for diagnosis, and management of upto 25 medical conditions.
Glucose:
Glucose is not normally present in the urine.
Once the level of glucose in the blood reaches a renal threshhold, the kidneys begin to excrete it into the urine in an attempt to decrease the blood concentration. So high blood concentrations lead to glucosuria, as does conditions that may reduce this renal threshold.
- Diabetes
- Liver disease
- Medications such as tetracycline, lithium, penicillin, cephalosporins
- Pregnancy
Bilirubin:
Produced as a by-product during the degradation of RBC in the liver and normally excreted in the bile. Once in the intestine it is excreted in the faeces (as stercobilin) or by the kidneys (as urobilinogen).
Presence of bilirubin in the urine may therefore indicate:
- liver disease
- biliary tract infection
- pancreatic causes of obstructive jaundice
Ketones:
Not normally found in the urine, ketones are produced during fat metabolism.
Presence of ketones may indicate:
- diabetes
- alcoholism
- eclampsia
- a state of starvation
- pregnancy
Specific Gravity:
The specific gravity (SG) of urine signifies the concentration of dissolved solutes and reflects the effectiveness of the renal tubules to concentrate it ( when the body needs to conserve fluid). If there were no solutes present the urines SG would be 1.000, the same as pure water.
The SG of urine is around 1.010 but can vary greatly:
Decreased SG may be due to:
- Excessive fluid intake (oral or IV fluids)
- Renal failure
- Acute golmerulonephritis, pyelonephritis, acute tubular necrosis
- Diabetes insipidus
Increased SG may be due to:
- Dehydration due to poor fluid intake, vomiting or diarrhoea
- Heart failure
- Liver failure
- Inappropriate antidiuretic hormone secretion
It also reflects a high solute concentration which may be from glucose (diabetes or IV glucose) or protein.
Blood:
Classified as microscopic or macroscopic haematoria. Microscopic means that the blood is not visible with the naked eye.
Blood may be present in the urine following trauma, smoking, infection, renal calculi or strenuous exercise.
It may also be present with:
- Urinary tract infections.
- Damage to the glomerulas or tumours which erode the urinary tract.
- Acute tubular necrosis.
- Traumatic catheterization.
- Damage caused by the passage of kidney stones.
- Contamination from the vagina during menstruation
The presence of myoglobin (myoglobinuria) after muscle injury will also cause the reagent strip to indicate blood.
pH:
Measures the hydrogen ion concentration of the urine.
It is important that a fresh sample be used as urine becomes more alkaline over time as bacteria convert urea to ammonia (which is very alkaline).
Urine is normally acidic but its normal pH ranges from 4.5 to 8.
Low pH (acidic):
- Foods such as acidic fruits (cranberries) can lower the pH, as can high a high protein diet.
- As urine generally reflects the blood pH, metabolic or respiratory acidosis can make it more acidic.
- Other causes of acidic urine include diabetes, diarrhoea and starvation.
High pH (alkaline):
- Low carb or vegetarian diet
- May be associated with renal calculi.
- Respiratory or metabolic alkalosis
- Urinary tract infection
Protein:
This is measuring the amount of albumin in the urine. Normally there should be no detectable quantities.
Elevated protein levels are known as proteinuria. Albumin is one of the smaller protiens, and if the kidneys begin to dysfuncion it may show an early sign of kidney disease.
Other conditions which may lead to protein in the urine include:
- Injury to the urinary tract, bladder or urethra
- Inflammation, malignancies.
- Multiple myeloma
Urobilinogen:
Normally present in the urine in small quantity. Less than 1% of urobilinogen is passed by the kidneys the remainder is excreted in the faeces or transported back to the liver and converted into bile.
Raised levels may be due to:
- Cirrhosis
- Hepatitis
- Hepatic necrosis
- Haemolytic and pernicious anaemia
- Malaria
Leukocytes:
Detects white cells in the urine (pyuria) which is associated with urinary tract infection.
Source: ImpactedNurse
Urinalysis may be useful in investigations and management of the following conditions.
2. Cirrhosis of the liver
3. Hepatitis
4. Hemolytic anemia
5. Malaria
6. Pre-eclampsia
7.Metabolic acidosis and alkalosis
8. Respiratory acidosis and alkalosis
9. Diabetse mellitus
10. Diarrhoea
11. Starvation
12. Renal calculi
13. Diabetes ketoacidosis
14. Biliary tract infections
15. Obstructive jaundice
16. Pregnancy
17. Alcoholism
18. Dehydration
19. Heart failure
20. Diabetes Insipidus
21. Nephropathy – Diabetic and Hypertensive
22. Multiple Myeloma
23. Menstruation
24. Vomitting
25. Cancers of the urinary tract, kidney, bladder
- Mayo Clinic article on Urinalysis
- Emergency Medicine News article on Urine dipstick testing
- Patient.co.uk article on Urine dipstick analysis
- “The Abnormal Urinalysis”, Pediatric Clinics of North America
—————end email uchek——————–
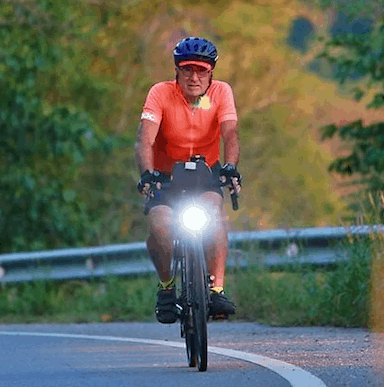

so your iphone is the test strip… would love to test for diabetes and dehydration
Nope you don’t pee on the iPhone 🙂 The iPhone camera takes a picture of the test strip yo have peed on and checks the colours.
It implies it measures specific gravity (dehydration as density increases) and sugar (maybe diabetes) although just tasting the sweetness of the urine can do that see http://en.wikipedia.org/wiki/Uroscopy
i may do some silly things but tasting my urine is not one of them 🙂